Het sturen op IC-capaciteit
De lockdown had ten doel om binnen de IC-capaciteit te blijven en dat is goed geslaagd. De IC-ers hebben zich wel drie slagen in de rondte moeten werken en doen dat nog steeds. Op de radio werd gemeld da ze zelfs 200% shifts draaien – dat was misschien spreekwoordelijk maar het geeft wel een indruk. En ze staan niet alleen. We staan met zijn allen solidair achter ze: andere patiënten worden naar achteren geschoven, afdelingen worden vrijgeruimd, bedrijven gaan ten onder, werkloosheid stijgt, miljarden verdampen zodat de IC zijn werk kan doen. Er wordt keihard gewerkt en des te frusterender moet het zijn om te zien dat zoveel van hun patiënten het toch niet redden.
Vanuit de zorgverlenend perpectief is dit niet meer dan logisch. Immers de IC is -naast andere dingen- ook een laatste redmiddel als verder niets helpt en een patiënt heeft het gevoel dat hij niet meer kan ademen. Ook als hij dat wel kan maar zijn longen halen geen zuurstof meer uit de lucht, is een arts het aan zijn taak en zijn stand verplicht om bij elke patiënt het onderste uit de kan te halen. Zelfs in bijna uitzichtloze situaties moet een arts kunnen volhouden, tot kansloze behandelingen in de IC aan toe. Dat is bewonderenswaardig en tegelijkertijd zou je artsen tegen zichzelf moeten beschermen. Ze zouden ongetwijfeld meer kunnen betekenen voor meer patiënten.
Sinds enige weken zien we ongeveer wat die op overvolle toeren draaiende IC tot dusver heeft betekend. De mortaliteit van corona is dankzij de IC verlaagd met ééntiende procent: 0,1%. Dat betekent: 1 op de 1000 corona-besmette mensen is gered door de IC. Exacte cijfers heeft het RIVM niet -dat zijn we inmiddels gewend- maar het is volgens henzelf iets van 1,4% in plaats van 1,5% sterfte onder coronapatiënten, om en nabij. Of 1.1% in plaats van 1,2%. Dat is dus wel een effect. Mogen we ook gaan kijken hoe dat effect in relatie staat tot de inspanningen? Het is bijna heiligschennis maar ik waag het toch maar.
De succes rate van de IC-behandeling in getallen
Het sterftepercentage van corona-patiënten op de IC wordt weleens geschat op 20%. Helaas fluctueert dat rond voor corona-patiënten tussen de 65%-70%. De overlevingskans is dus ongeveer 1 op 3.
In Italië waren de resultaten nog veel slechter. Daar namen ze ook gemakkelijker kansloze patiënten op dan in Nederland. De horrorbeelden die we gezien hebben hadden voorkomen kunnen worden als er een leeftijdsgrens (en/of later: een BMI-grens) was gehanteerd. Als Italië wat striktere richtlijnen had gehanteerd, dan hadden kansrijke patiënten die nu op de gang zijn gestorven nog een kans gehad. In Italië was het meer een veredeld hospice. Daar hadden ze de capaciteit niet voor.
Nederland, 22 april
[28-4: getallen zijn hoger, kernpunt nog steeds geldig]
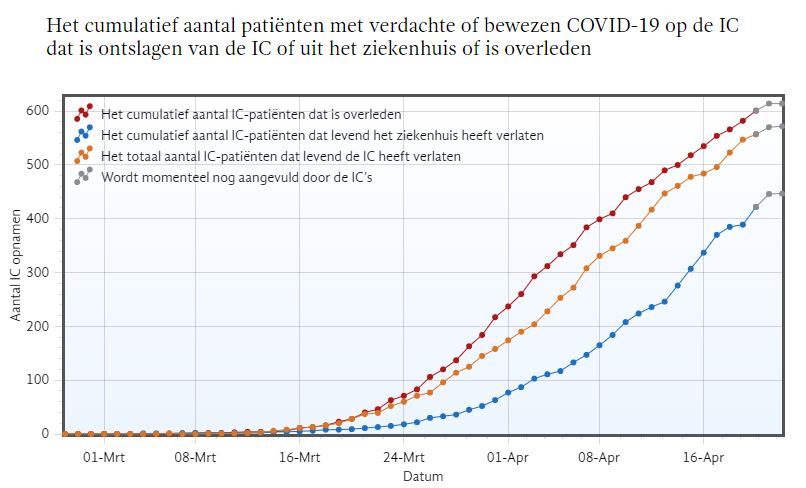
In de afgelopen 6 weken zijn er 2680 IC-patiënten opgenomen [28-4: 2773]. Daarvan lagen er op 22 april nog 965 op de IC [28-4: 788]. Van de overige 1715 ex-IC-patiënten [28-4: 1985] zijn er 572 [28-4: 625] levend* van de IC afgekomen (inderdaad: 33%). De gegevens komen van de Stichting Nederlandse Intensive Care Evaluatie. Hoeveel van deze patiënten later alsnog overlijdt is niet bekend.
De blauwe lijn geeft aan dat er minder mensen levend het ziekenhuis verlaten dan dat er levend uit de IC komen. Maar hier speelt de vertraging ook een rol en we weten ook niet hoe lang IC-patiënten gemiddeld nog in het ziekenhuis verblijven. Dus vanwege (opnieuw) de incompleetheid van de data laten we dit maar buiten beschouwing.
Bron (dd 22 april): Nationale Intensive Care Evaluatie
Er zijn ongeveer 550.000 mensen besmet met het virus. (bron dd 16 april: Sanquin Hotels) Vandaar dat de 572 geredde IC-patiënten staan voor 0,1% van de mortaliteit onder besmette personen. De aanname is daarbij dat de IC-overlevenden het zonder IC niet zouden hebben gered, dus dat bijvoorbeeld een (thuis)behandeling met medicatie en zuurstof niet zou hebben geholpen.
De mogelijkheid dat de beademing de toestand van veel patiënten heeft verergerd laat ik verder buiten beschouwing. Daar zijn aanwijzingen voor maar dat is op dit moment ook alles.
Conclusion
Als niet-medicus en niet-econoom zou ik graag horen dat de behandeling bijdraagt aan de volksgezondheid en betaalbaar is conform de gangbare normen of misschien 2x de gangbare normen. Mijn voornaamste reden om dit stukje te schrijven is dat overwegingen zoals deze buiten beschouwing lijken te blijven.
Deze relativering leest misschien als een rechtstreekse aanval op alles wat met IC te maken heeft. Dit is nadrukkelijk niet de bedoeling. Wat wel de bedoeling is: de beleidsfocus op de IC en wat daarvoor in de strijd wordt gegooid vereist een voortdurende evaluatie van onze targets, onze performance en de ROI in termen van volksgezondheid en welzijn. Ik heb nog geen spoor van een evaluatie gezien.
Een nog wat scherper gedachtenexperiment: stel dat er een farmaceut met een corona-middel zou komen, ‘FiniCor’…
NIEUW! FINICOR!
De kuur die bewezen een einde maakt aan al uw corona-klachten!
- Slaat geen enkele corona-behandeling aan? Dan komt u automatisch in aanmerking voor de Finicor kuur!
- FiniCor wordt alleen verstrekt aan patiënten die in het ziekenhuis ondanks medische zorg blijven verslechteren. Finicor is bewezen effectief bij 33% van deze patiënten. Degenen waarbij het middel niet aanslaat (ongeveer tweederde) zullen helaas alsnog komen te overlijden.
- De kuur duurt ca. 3 weken. Na een behandeling met FiniCor is een intensieve revalidatieperiode gewenst. Deze kan soms tot 2 jaar duren.
- De productiecapaciteit voor FiniCor is beperkt. Om aan de vraag te kunnen voldoen zal het land in lockdown moeten. Dit beperkt de snelheid van immunisatie zodat de leveringen over een langere periode kunnen worden verdeeld.
Zou dit middel op de markt komen?
Geld is niet alleen ‘geld’. Het staat ook voor cultuur en zorg.
Dan ook nog even een financiële overdenking: de miljarden die nu worden geïnvesteerd zullen later vooral ten koste gaan van de collectieve voorzieningen zoals cultuur en gezondheidszorg. Gezondheidszorg is daarvan misschien wel de belangrijkste (zeg ik als muziekmaker).Tekorten in de zorgbudgetten zullen ten koste gaan van de volksgezondheid. Ik heb zelf niet de expertise om te berekenen hoe elk miljard minder zich vertaalt in ziekte en sterfte. ‘Poverty kills’, dat wijzen de cijfers wel uit, maar meer weet ik niet. Het scenario waarin de gezondheidszorg zelf aan de beademing moet is echter niet zo moeilijk voor te stellen.
Ik zou dus graag zien dat de discussie wordt gevoerd over wanneer we moeilijke beslissingen gaan nemen, nu of in de toekomst als het geld op is? Op dit moment hebben we nog opties maar dan, na de crisis, staan we voor een fait accompli dat mogelijk veel meer mensenlevens gaat kosten dan we gered hebben. Dan hebben we ‘Spijt achteraf om wat we nu nagelaten hebben’, om met Rutte te spreken.
*Levend van de IC: Daarbij is een minderheid van de overlevenden na een paar maanden weer aardig op de been. Het merendeel is er niet best aan toe met blijvende longschade en/of psychische trauma’s. Niemand kijkt raar op van een revalidatie van twee jaar. Lang niet alle ex-IC-ers kunnen daarna hun voormalige leven hervatten.