Tweaking the lockdown always focuses on the available ICU capacity. After all, insufficient ICU capacity leads to disastrous consequences for public health. A few months ago, we played it safe with that starting point. There is now more data. Progressive insight raises new questions. What disastrous consequences are we actually talking about? And is that worse than the socio-economic disaster that is now unfolding? How can you convert deaths to public health? These are questions that model builders don't hear themselves ask, but we do.
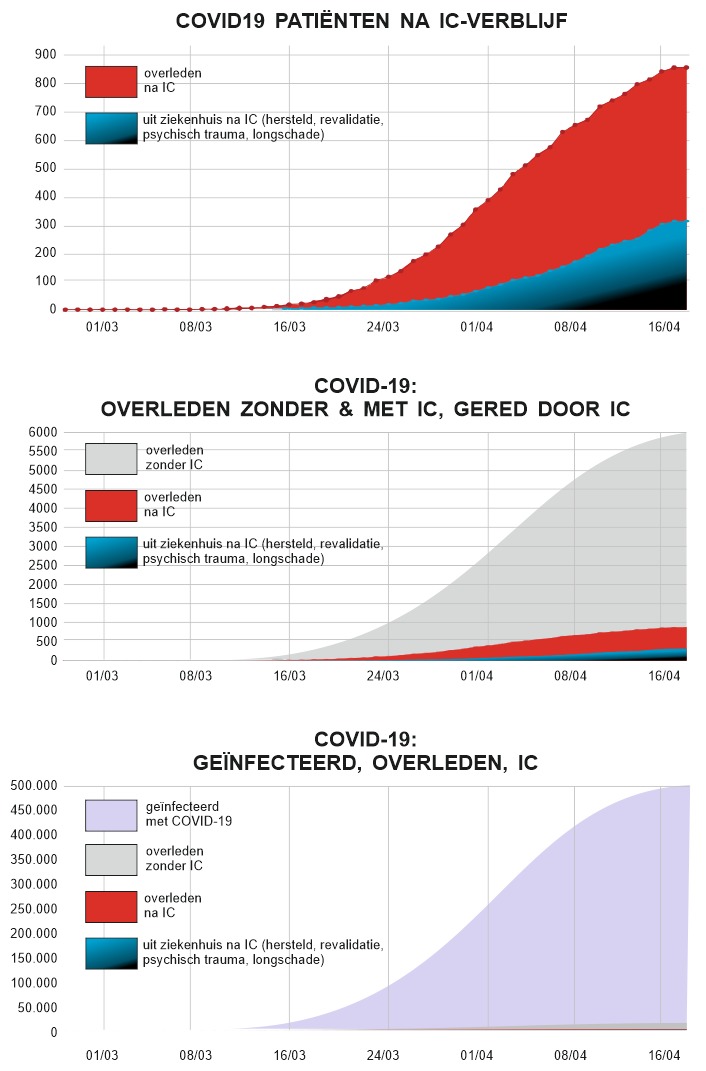
I visualized some key figures to gain insight into the importance of the ICU and to what extent it could affect the mortality rate. It is a rough visualise, but the figures come from Statistics Netherlands, RIVM and the National Intensive Care Evaluation Foundation.
Three pictures:
- Treatment results in the ICU
- ICU results related to total mortality
- ICU results related to total number of sick (infected).
The fourth picture I had in my head is pointless because there is nothing left to see on it. That picture would compare this with Public Health: 17 million Dutch people. And then juggling with QALY-like weighings also comes into play. 17 million people have an average of 40 years to go, which is 17Γ40 = 680 million years of life. But let's say that only the next 5 years will be ruined (according to many, an underestimate). That then stands for 17 million x 5 = 85 million years of impaired well-being and deteriorated facilities and health.
So if, for example, we save 850 corona victims in the ICU (of people who have an average of less than 10 years to live in questionable health, after such ICU treatment), then every life saved has ruined about 100,000 years of well-being.
It remains an impossible decision, but we will have to do something with it.

0 reactions